-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Michel Goldberg*
Corresponding Author: Michel Goldberg, Department of Oral Biology, Faculty of Fundamental and Biomedical Sciences, INSERM UMR-S1124, Paris Cité University, France.
Received: May 11, 2023 ; Revised: May 15, 2023 ; Accepted: May 18, 2023 ; Available Online: May 31, 2023
Citation: Goldberg M. (2023) Gerontopsychiatry. J Oral Health Dent Res, 3(3): 1-3.
Copyrights: ©2023 Goldberg M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Depression in old adults, and panic anxiety disorder, are the main characteristics of gerontopsychiatry. Interactions between dementia, panic hallucinations and delusions, psychotic disorders, drugs, insomnia, suicide and dementia, define the psychiatric aspects of old patients. Bipolar troubles, and mental disorders are typical for psychiatry of old patients. Starting at 65 years and/or older, interactions between drugs, polymerization, and schizophrenia provide substantial evidences of psychic disorders. Dementia, neuropsychiatric complications, suicidal thinking, medical psychiatric disorders characterize psychiatric conclusive evidence in the elderly. Drugs, such as anticholinergics, antiparkinson, steroids and beta-blockers, as well as alcohol and benzodiazepine withdrawal, may produce mental health disorders. Psychiatric alterations have consequences that include social deprivation, poor quality of life, cognitive decline, disability, increased risks for somatic disorders, suicide, and increased non-suicidal mortality. Geriatric psychiatrics aiming to investigate the causes of neurologic effects, are symptoms that should be treated by an alienist.
Keywords: Gerontopsychiatry, Polymedication, Suicidal thinking, Dementia, Schizophrenia, Bipolar trouble, Depression, Elderly patients
GERONTOPSYCHIATRY
In the elderly, psychiatric disorders include depression, anxiety disorders, and psychosis. In the aged patients they are related to diseases. Psychiatric disorders involve, suicidal thinking, and increased non-suicidal mortality [1].
In the last 60 years, the number of adults over 65 has grown extensively. Hence, the needs for geriatric psychiatry have considerably increased. Depression occurs when old patients are stopping work, have less money and more health problems. They are affected by the death of partners or friends. They lose interest in life, feel tired, loose appetite and weight, find had to relax, want to avoid people, feel irritable, and that cannot concentrate properly, and loose sexual feelings.
Gerontopsychiatry involves
Gerontopsychiatry starting at 65 years or beginning earlier: it implicates schizophrenia and/or bipolar troubles.
For older patients (more than 65 years), they display forms of schizophrenia or/and depression.
For hospitalized patients, 1 to 4% aged persons are depressed or bipolar. They display severe symptoms and risks of suicide.
Medications favor depressed symptoms: especially psychotrops (e.g. benzodiazepins).
There is a lack of convergence between psychiatric diagnostic and psychotropic treatment.
For older patients, hospitalized for more than 3 months, there is a risk of interaction between drugs, polymedication and schizophrenic troubles. Some patients are bipolar, displaying phobic troubles and they need to be treated by an alienist.
Low energy, sadness, loss of interest for diverse activities and social handicaps, professionals and affective disturbances. Bipolar troubles may be responsible for suicide. It is the second pathology leading to suicide after mental anorexia.
Insomnia of the patients, with a lake of being tired. Bipolar troubles are energetic, with an enhanced libido.
Ionogramme: reveals kaliemia, calcemia, urea, creatinine.
NFS, platelets, CRP, TSH.
Urines analysis indicate the use of cannabis, cocaine, opium, and amphetamines.
Scanner or IRM, and ECG support this assumption.
Drugs treatments: lithium, valpronate, antipsychotic of the 2d generation (Olanzapine, Risperidone, QueDiseases tiapine, Aripiprazole and selective inhibitors of recapture of serotonin (ISRS).
Some antidepressants have side effects: such as dry mouth, and/or interference with other medicines.
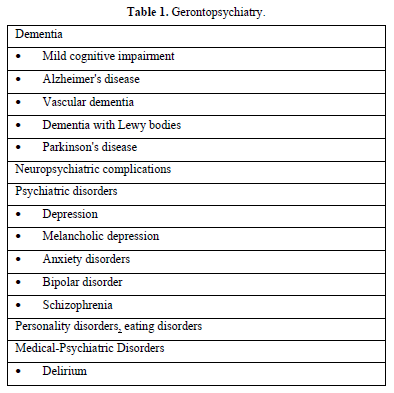
Gerontopsychiatry implicates oral and mental troubles, and constitutes the framework of psychic alterations (Table 1).
Anxiety disorders, somatic symptom disorders (hypochondrostasis), confused thinking is frequent in old patients. They display reduced ability to concentrate, sadness, tiredness, low energy, sleeping problems. The sick patients display hallucinations. They overuse drugs. They display excessive anger. Hostility, and violence are frequent. Suicidal thinking is the most frequent aspect of the pathology of old patients.
CONCLUSIONS
Gerontopsychiatry is dealing with prevention of sickness for humans in old age: dementia, memory problems, fear of death for men. For women, the symptoms include perinatal depression, perimenopause-related depression, identity crisis and menopause. Both of they constitute the most numerous diseases grouped in gerontopsychiatry. Phobic troubles, and suicide risks, all of them need to be adequately managed by an alienist.
No Files Found
Share Your Publication :